Introduction
Kidney disease is a serious condition affecting millions of people worldwide. The kidneys play a crucial role in filtering waste, balancing electrolytes, regulating blood pressure, and supporting overall health. When kidney function is impaired, toxins and excess fluids accumulate in the body, causing complications that can affect the heart, bones, blood, and nervous system.
Chronic Kidney Disease (CKD) develops gradually over years, often without noticeable symptoms in its early stages. This silent progression makes early detection essential. Worldwide, CKD has become a major health challenge due to rising rates of diabetes, hypertension, and aging populations. Understanding the causes, symptoms, risk factors, and management strategies for kidney disease is essential for prevention and maintaining long-term health.
Anatomy and Function of the Kidneys
The kidneys are two bean-shaped organs located on either side of the spine, just below the rib cage. Each kidney contains over a million tiny filtering units called nephrons, which are responsible for:
-
Filtering blood to remove waste and excess fluid
-
Balancing electrolytes like sodium, potassium, and calcium
-
Regulating blood pressure through hormone production
-
Stimulating red blood cell production via erythropoietin
-
Maintaining bone health by activating vitamin D
Healthy kidneys are essential for survival, and their gradual deterioration can have far-reaching consequences.
What is Kidney Disease?
Kidney disease refers to the gradual loss of kidney function over time. It can be categorized as:
- Chronic Kidney Disease (CKD): Long-term progressive decline in kidney function, often caused by diabetes or high blood pressure.
- Acute Kidney Injury (AKI): Sudden kidney damage due to infection, injury, or medication, which may be reversible.
- Inherited Kidney Disorders: Conditions like polycystic kidney disease, which cause structural damage to the kidneys.
When kidney function drops below a critical threshold, waste accumulates in the body, leading to kidney failure (end-stage renal disease), which requires dialysis or a kidney transplant.
Stages of Chronic Kidney Disease
CKD is classified into five stages based on eGFR (estimated glomerular filtration rate), which measures kidney function:
| Stage | eGFR (mL/min/1.73 m²) | Description |
|---|---|---|
| 1 | ≥90 | Kidney damage with normal function |
| 2 | 60–89 | Mild decrease in function |
| 3a | 45–59 | Mild to moderate decrease |
| 3b | 30–44 | Moderate to severe decrease |
| 4 | 15–29 | Severe decrease in function |
| 5 | <15 | Kidney failure (requires dialysis or transplant) |
Understanding the stage of CKD is essential for treatment planning and preventing complications.
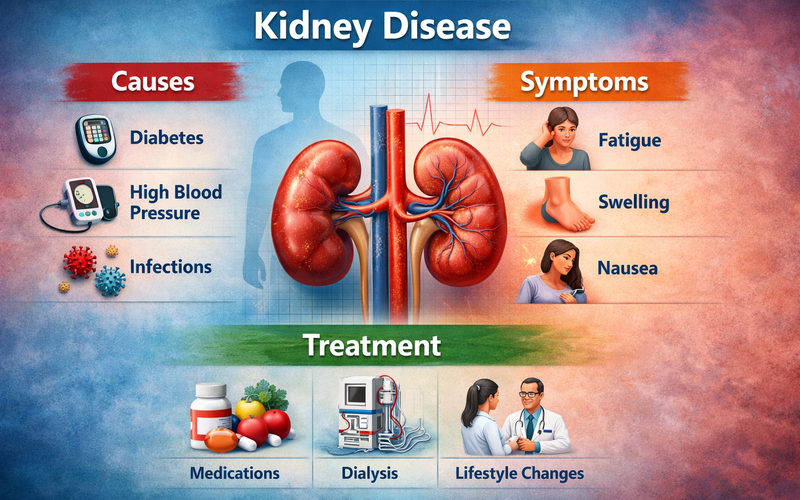
Kidney Disease Causes and Risk Factors
1. Diabetes
High blood sugar levels damage the nephrons over time, making diabetes the leading cause of CKD globally.
2. High Blood Pressure
Uncontrolled hypertension damages kidney blood vessels and accelerates kidney function decline.
3. Heart Disease and Obesity
Heart conditions and excess body weight increase the risk of CKD through inflammation, high blood pressure, and insulin resistance.
4. Smoking and Unhealthy Lifestyle
Smoking reduces blood flow to the kidneys, while excessive alcohol and certain medications (like painkillers) contribute to kidney damage.
5. Age
Kidney function naturally decreases with age, making older adults more susceptible.
6. Genetics and Medical Conditions
Polycystic kidney disease, lupus, and recurring urinary tract infections increase the likelihood of CKD.
Symptoms of Kidney Disease
Early CKD often has no symptoms, but as kidney function worsens, signs may include:
-
Fatigue and weakness
-
Swelling in the legs, ankles, or face
-
Dry, itchy skin
-
Nausea, vomiting, and loss of appetite
-
Changes in urination (frequency, foaming, or blood in urine)
-
Shortness of breath
-
Persistent high blood pressure
-
Sleep disturbances
Because symptoms are subtle, regular screening for high-risk individuals is critical.
Complications of Kidney Disease
CKD can lead to multiple systemic complications:
-
Cardiovascular disease: Increased risk of heart attack and stroke
-
Anaemia: Reduced red blood cell production leading to fatigue
-
Bone disease: Loss of calcium and vitamin D metabolism
-
Fluid retention: Swelling and pulmonary complications
-
Hyperkalaemia: High potassium levels affecting heart rhythm
-
Neuropathy: Nerve damage causing pain or tingling
Diagnosis
Early detection depends on a combination of tests:
Blood Tests
-
eGFR: Assesses kidney filtering capacity
-
Creatinine: Elevated levels indicate reduced kidney function
Urine Tests
-
Albumin-to-creatinine ratio: Detects protein leakage
-
Urinalysis: Identifies blood, sugar, or infection
Imaging
-
Ultrasound or CT scan: Checks kidney size and structure
-
Biopsy: Confirms cause in uncertain cases
Screening is especially important for patients with diabetes, hypertension, or a family history of kidney disease.
Kidney Disease Treatment Options
While CKD cannot usually be reversed, early intervention slows progression:
1. Manage Underlying Causes
-
Diabetes management through medication, diet, and exercise
-
Blood pressure control using ACE inhibitors or ARBs
2. Lifestyle Changes
-
Low-sodium, moderate-protein diet
-
Regular physical activity and weight management
-
Quit smoking and reduce alcohol intake
3. Treat Complications
-
Medications for anaemia, bone disease, fluid retention, and cholesterol
-
Monitor electrolytes regularly
4. Advanced Treatments
-
Dialysis: Mechanical filtration of blood
-
Kidney transplant: Replacement of non-functional kidney
Kidney Disease Prevention Strategies
Preventing kidney disease is achievable with lifestyle and medical care:
- Maintain healthy blood sugar and blood pressure
- Stay hydrated and avoid excessive processed foods
- Avoid smoking and limit alcohol
- Exercise regularly and maintain a healthy weight
- Routine screening for high-risk individuals
Early prevention reduces the risk of kidney failure and complications significantly.
Kidney Disease Dietary Considerations
Diet plays a critical role in managing CKD:
-
Low sodium: Helps reduce fluid retention
-
Controlled protein intake: Reduces kidney workload
-
Potassium monitoring: Important in advanced CKD stages
-
Phosphorus limitation: Protects bones
-
Hydration: Adequate water intake without overloading the kidneys
Consulting a dietitian for a personalized plan is recommended for all CKD patients.
Emerging Research and Future Treatments
-
Artificial intelligence and predictive models are improving early detection
-
New medications show promise in slowing CKD progression
-
Regenerative medicine and kidney bioengineering could transform treatment in the future
Frequently Asked Questions (FAQs)
Q1: Can kidney disease be reversed?
Early-stage CKD cannot usually be reversed, but its progression can be slowed significantly with treatment and lifestyle changes.
Q2: How often should I screen for CKD?
High-risk individuals should have blood and urine tests at least annually, or more frequently if recommended by a doctor.
Q3: Is dialysis the only option in late-stage CKD?
Yes, in kidney failure, dialysis or kidney transplant is required to sustain life.
Q4: Can diet alone prevent CKD?
Diet helps, but controlling underlying conditions like diabetes and hypertension is equally crucial.
Q5: Are herbal supplements safe for kidney health?
Some herbal remedies can harm kidneys, so always consult a healthcare professional before use.
Conclusion
Kidney disease is a silent yet serious condition that requires awareness, early detection, and proactive management. By understanding the causes, recognizing subtle symptoms, adopting a kidney-friendly lifestyle, and seeking timely medical care, individuals can protect kidney health and improve overall well-being.
Key Takeaways:
- Early detection saves lives
- Manage diabetes and blood pressure
- Maintain a healthy lifestyle and diet
- Monitor kidney function regularly
Taking control today can prevent long-term complications and ensure healthy kidney function for years to come. Visit my site.